The US prepares to end its Covid-19 PHE – what medical device manufacturers should know
The US Covid-19 public health emergency (PHE) is set to end on 11 May 2023. The PHE was initially declared in early 2020 and has been renewed every 90 days since. However, following the last renewal in January 2023, President Biden announced that there would be no further extensions.
Given the regulatory flexibilities that were introduced in response to the pandemic, the impending end of the PHE has naturally led to questions around the impact for medical device manufacturers. In this post, we discuss which flexibilities will be impacted by the PHE ending and the next steps that should be taken by manufacturers.
Emergency Use Authorisations (EUAs)
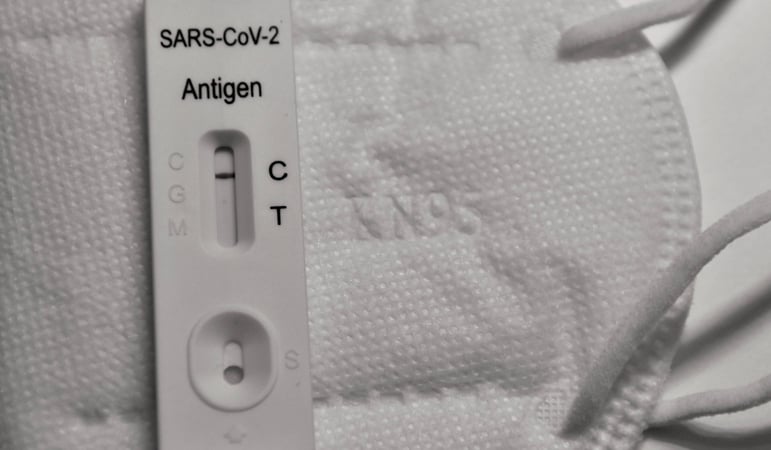
Emergency Use Authorisations were introduced for a number of products (including Covid-19 test kits, respiratory protective equipment and certain ventilators) at the start of the pandemic. EUAs allow these products to be marketed in the US based on best available evidence, without other evidence that would typically be required for device approval/clearance.[1] The purpose of these EUAs was to expedite the regulatory approval process for devices needed to help combat the pandemic.
The end of the PHA does not directly impact these EUAs. Instead, for an EUA to be terminated, the HHS Secretary must make a separate determination that the circumstances justifying the emergency use no longer exist. Each EUA is to be terminated individually by the HHS Secretary. Once a determination has been made that an EUA is to be terminated, manufacturers will be given 180 days advance notice during which they should submit applications for FDA clearance/approval if they wish to continue marketing their devices.
The HHS Secretary has not yet started terminating EUAs issued as a result of the pandemic (although several have been revoked, usually in response to voluntary requests from manufacturers). However, manufacturers who are currently making use of Covid-19 related EUAs should be aware of the likelihood of their authorisations terminating at some point in the near future. While the end of the PHA will not directly invalidate any EUAs itself, the announcement is indicative of a more general scaling back of the regulatory flexibilities introduced as a result of the pandemic.
To prepare, manufacturers should consider starting the process of pulling together their regulatory submissions. The FDA recently announced its authorisation of the first Covid-19 Antigen Test using the traditional premarket approval pathway. This means that Covid-19 test devices (the device type most commonly granted EUAs) now have a clear predicate on which manufacturers can base their 510(k) applications. The availability of this predicate will significantly lower the cost and timeline for obtaining full regulatory clearance/approval for Covid-19 tests which had previously relied upon EUAs.
Enforcement discretion policies
One area where the end of the PHA will have a direct impact is in relation to FDA enforcement discretion policies. The Agency issued these policies, usually in the form of guidance documents, to facilitate the availability of devices used to diagnose, treat and prevent Covid-19.[2] The FDA has indicated that it does not intend for all of its enforcement discretion policies to be impacted immediately by the end of the PHE. Instead, it plans to publish a notice regarding which policies are to be temporarily extended and which will be allowed expire. Since the FDA has yet to publish this notice, the exact impact of the end of the PHE on enforcement discretion policies is yet unknown.
However, some guidance can be taken from the FDA's draft document “Transition Plan for Medical Devices That Fall Within Enforcement Policies Issued During the COVID-19 Public Health Emergency” (issued December 2021). This document highlights various enforcement discretion policies which were adopted specifically to support the response to the Covid-19 PHE. Therefore, it can be inferred that once the PHE ends, these policies will also be terminated. The policies listed in the document include those relating to remote digital pathology devices, imaging systems, non-invasive foetal and maternal monitoring devices and telethermographic systems, among others.
The draft document also states that manufacturers will have a buffer period of 180 days between the implementation date of the guidance and the final withdrawal of the enforcement discretion policies. Since the guidance document is still in draft form, it does not currently have an implementation date. However, with the upcoming end to the PHE, it is likely that one will be announced soon. Once the implementation date has been established, manufacturers will have 180 days to bring their products into compliance with the standard regulations for medical devices.
How we can help
Regtik, our healthcare regulatory explorer tool, can help you navigate the legal maze by walking your product through a series of simple questions designed to determine which rules and regulations are applicable It is able to provide results for various jurisdictions (the US, EU, UK and Australia) in one single assessment and can be used multiple times on different versions of your product.
If you are interested in learning more about Regtik or would like to request a demo, please contact any member of our team or register your interest below.
[1] FDA, Understanding the Regulatory Terminology of Potential Preventions and Treatments for COVID-19
[2] The policies adopted a wide variety of measures, including relaxing the FDA’s inspection practices, altering FDA’s supply chain disruption reporting requirements, and exercising enforcement discretion to permit the marketing of certain unapproved or otherwise non-compliant products during the PHE




